Supporting Children and Young People with Anxiety
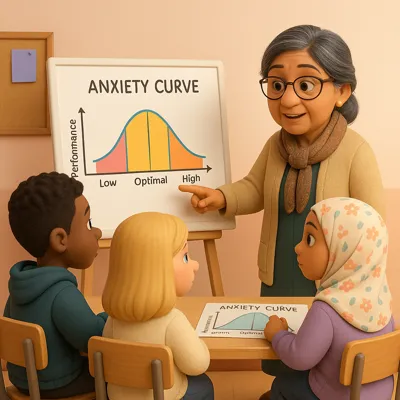
The Yerkes-Dodson Law (Yerkes and Dodson, 1908), also known as the anxiety curve, is a psychological concept that illustrates how levels of anxiety or arousal affect performance.
This is especially relevant in SEMH settings because it helps us understand how anxiety can directly affect a young person’s ability to engage, learn, and cope with everyday situations.
Many SEMH pupils live in a state of high anxiety; this could be due to neurodivergence, past traumas or unstable home environments, leaving them in a constant state of alert.
Before we delve further into the anxiety curve, let’s gain a clearer understanding of anxiety.
What is Anxiety and What Does Anxiety Feel Like?
Anxiety is a natural response to stress or perceived danger. It is a feeling of unease, encompassing worry, fear, or nervousness, and is something that everyone experiences occasionally.
Anxiety can manifest through a variety of symptoms, including physical, emotional, cognitive, and behavioural symptoms.
- Physical symptoms: racing heart, rapid breathing, sweating, shaking, and stomachaches.
- Emotional symptoms: feelings of tension, restlessness, or fear that something terrible is about to occur.
- Cognitive symptoms: overthinking, difficulty concentrating, and imagining worst-case scenarios.
- Behavioural symptoms: avoiding people, places, or situations that trigger fear.
Why Do Children Get Anxious?
Anxiety is a component of the “Fight, Flight, or Freeze” response (Siegel, 2012), which our brain activates when it perceives danger. During this period, the rational part of the brain shuts down, while the primal or survival part takes control, focusing solely on keeping you safe.
When anxiety arises too frequently or intensely, particularly without a real threat, it can become overwhelming or even lead to a mental health issue.
How Might This Present in Children and Young People?
The way adults experience anxiety may differ from how children show it; therefore, it is essential to recognise the following signs that may indicate a child or young person is feeling anxious.
Emotional Signs
- Constantly seeking reassurance (e.g., "What if...?" questions)
- Becoming easily upset, tearful, or appearing overwhelmed by minor changes
- Experiencing an intense fear of failure or making mistakes
Cognitive Signs
- Difficulty concentrating or appearing "disengaged"
- Perfectionism or becoming paralysed during tasks
- Harsh self-talk (“I can’t do it,” “I’m not smart”)
Behavioural Signs
- Refusal to attend school or participate in activities
- Avoidance behaviours (e.g., frequently needing to use the restroom, requesting to leave the classroom)
- Angry outbursts or aggression when feeling anxious (fight response)
- Withdrawing, becoming quiet or "invisible" (freeze response)
Physical Symptoms
- Complaints of headaches, stomachaches, or nausea
- Fidgeting, nail-biting, or skin-picking
- Panic-like symptoms (e.g., rapid breathing, flushed face, trembling)
What This Might Look Like in SEMH Pupils
- A pupil suddenly flips a table during a difficult task—not merely "bad behaviour," but possibly a sign of panic.
- Another student constantly doodles or asks to assist the teacher—they might be masking (Treisman, 2017) anxiety with distraction or a desire to please others.
- A child who never submits work might be so anxious about failing that they’d prefer not to try.
The Anxiety Curve
The anxiety curve illustrates the relationship between anxiety and performance, divided into three zones:
- Low anxiety → Low performance (boredom, lack of motivation)
- Moderate anxiety → Peak performance (alert, focused, motivated)
- High anxiety → Low performance (panic, overwhelm, shutdown)
The anxiety curve illustrates how a moderate amount of pressure can motivate us to take action, while excessive stress can lead children to freeze, lash out, or avoid situations.
Children with SEMH needs often find themselves in the high-anxiety/low-performance zone; this is not a sign of laziness but rather a result of their nervous systems being overwhelmed.
Examples in Practice
The table below provides examples of what children in Low, Moderate, and High zones of the anxiety curve might experience in various scenarios
Task: A pupil is asked to join a group project
| How it looks | |
|---|---|
| Low | “Whatever,” they act like they don’t care or isolate themselves |
| Moderate | They feel somewhat uncertain but join in and contribute. |
| High | They say something rude, try to control the group, or walk off due to social stress. |
Task: Emotional Check-In
| How it looks | |
|---|---|
| Low | Appears flat or unengaged, says “I’m fine” with little emotion. |
| Moderate | Openly shares some feelings with a trusted adult |
| High | Avoids eye contact, deflects questions, or becomes defensive or angry. |
Task: PE Activity
| How it looks | |
|---|---|
| Low | “I don’t want to play”—no interest, wandering off. |
| Moderate | They feel energised, work with peers, and enjoy the game. |
| High | They become hyper-competitive, argue with teammates, or refuse to join. |
Task: Presenting in front of the class
| How it looks | |
|---|---|
| Low | The pupil is disengaged and shrugs it off—“I don’t care.” |
| Moderate | They feel a bit nervous but motivated—"I want to do well." |
| High | They freeze, tear up, or walk out—“Everyone will laugh at me.” |
Task: A pupil is given a test.
| How it looks | |
|---|---|
| Low | They don’t try. |
| Moderate | They focus and do well. |
| High | They cry, refuse, or rip the paper up |
Signs to Look Out For at Each Stage
Here’s a breakdown of signs to look out for at each stage of the anxiety curve, especially in pupils with SEMH needs. These signs can help staff and caregivers identify where a pupil might be on the curve, and respond supportively:
| Stage | Emotional | Behavioural | Cognitive |
|---|---|---|---|
| Low Anxiety / Under-Aroused | Flat or indifferent mood / Low motivation or energy / Appears uninterested | Wandering around the room / Refusing to start tasks / Passive or avoidant | Struggles to get started / Easily distracted / Says "This is boring" or "What's the point?" |
| Moderate Anxiety / Focused Arousal | Calm but energised / Shows interest / Willing to try | Engaged in the task / Responds well to challenge / Flexible and cooperative | Can focus and process instructions / Makes an effort / Shows pride in their work |
| High Anxiety / Over-Aroused | Tearful, panicked, irritable / Easily frustrated or scared / Expresses self-doubt or catastrophising (“I’ll mess it up”) | Avoiding or fleeing the task / Meltdowns, aggression, or complete shutdown / Needing constant reassurance | Can’t focus or process / Gets stuck on small details / May freeze, rush, or give up quickly |
Anxiety in Children and Young People with SEMH
For many pupils with SEMH needs, particularly those who are neurodivergent or have experienced trauma, the anxiety curve differs from that of their neurotypical peers:
- Their baseline anxiety may be elevated due to a heightened stress response system (hypervigilance).
- A seemingly “small” demand can quickly push them into the high-anxiety zone.
- They may spend less time in the “optimal” part of the curve—not due to lack of capability, but because their nervous system constantly feels unsafe or dysregulated.
Anxiety Responses: Behaviour as Communication
Anxiety doesn’t always look like worry or panic:
- Some pupils mask—they smile, comply, or try to “blend in,” often at significant emotional cost. These pupils might seem “fine” in class but melt down later at home.
- Others may explode—shouting, throwing objects, or running away. These are not random outbursts, but rather fight-or-flight responses triggered by feelings of being overwhelmed, misunderstood, or unsafe.
Both masking and outbursts are protective strategies, not signs of defiance or manipulation.
Building Relationships: The Importance of Co-Regulation and Emotional Safety
Before we ask pupils to self-regulate, they need to experience co-regulation (Cozolino, 2013)—calm, emotionally present adults who model and share regulation.
Emotional safety (Cozolino, 2013) is key: predictable routines, warm relationships, clear boundaries, and a sense of being seen and accepted.
This helps shift the curve over time, reducing baseline anxiety and extending the window for learning and connection.
Supporting Children Around the Anxiety Curve

Helping children and young people move toward the optimal zone on the anxiety curve involves understanding what calms their nervous system, builds trust, and facilitates learning.
Here are key strategies to reduce anxiety and support regulation:
Predictability and Routine
- Pupils feel safer when they know what to expect.
- Use consistent routines, visual timetables, and give advance warnings of changes.
- Create structured environments with flexible scaffolding, not rigid control.
Emotion Coaching
- Help pupils label and understand what they’re feeling: “It sounds like you’re feeling frustrated because the work feels too hard.”
- Validate their emotional experience before moving to problem-solving.
- Use calm moments to reflect and teach emotional literacy, not during crisis.
Flexible Expectations
- Meet pupils where they are, not where we wish they were.
- Offer choices, break tasks into chunks, provide movement breaks, or adjust goals when anxiety is high.
- Flexibility isn’t lowering standards—it’s helping pupils access them safely.
Calm, Non-Reactive Adult Presence
- A dysregulated adult cannot regulate a dysregulated child.
- Stay grounded, speak slowly, reduce language, and model steady breathing.
- Use connection, not correction, as your first response.
When to Refer for Further Mental Health Support
Sometimes anxiety is persistent, severe, or linked to more profound needs. Consider a referral when:
- A pupil is frequently overwhelmed despite support.
- They show signs of panic attacks, phobias, or obsessive behaviours.
- Anxiety significantly impacts attendance, sleep, eating habits, and self-esteem.
Referral routes may include the school SENCO, CAMHS, an Educational Psychologist, or a trusted local mental health service.
Conclusion
Understanding the anxiety curve provides a powerful lens through which to view the behaviours and challenges of children and young people, especially those with SEMH needs. It reminds us that what may appear to be defiance, disinterest, or disengagement is often the visible manifestation of an overwhelmed nervous system.
When we recognise the signs of anxiety and understand where a pupil may sit on the curve, we are better placed to respond with empathy, flexibility, and support. Through predictable routines, emotional coaching, calm adult presence, and a focus on emotional safety, we can help pupils gradually shift toward the optimal zone, where learning, connection, and confidence can flourish.
Ultimately, the goal is not to eliminate anxiety altogether, but to create conditions where young people feel safe enough to stretch, try, and thrive. When we hold this understanding at the heart of our practice, we become not only educators but co-regulators, allies, and advocates in their journey toward resilience and wellbeing.